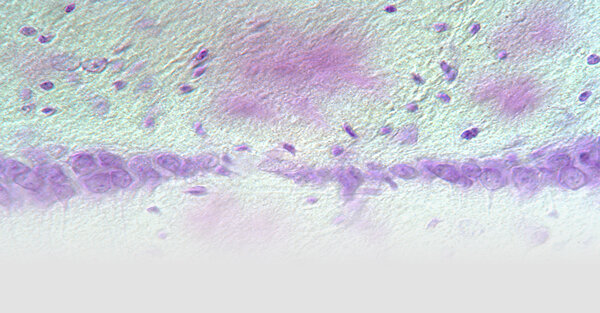

„Zerebrale Proteopathie" ist die Bezeichnung für neurodegenerative Erkrankungen, bei denen sich aggregierte Proteine abnorm im Gehirn anreichern. Die wohl bekannteste Proteopathie ist die Alzheimer-Krankheit, bei der sich fibrilläre Amyloid-β-Peptide (Aβ) extrazellulär in parenchymalen Plaques oder in den Gefäßen als zerebrale Amyloidangiopathie ablagern. Unser Ziel ist es, die zellulären und molekularen Mechanismen der Neurodegeneration und die pathogenen Proteine, die an der Entstehung der Alzheimer-Krankheit und der zerebralen Amyloidangiopathie beteiligt sind, besser zu verstehen.
Weitere Informationen zu den Zielen unserer Forschung, aktuellen Forschungsergebnissen, Mitarbeitenden und Publikationen finden Sie in englischer Sprache.
1. To understand how Aβ aggregation originates, spreads, and leads to neuronal dysfunction and dementia.
2. To study non-Aβ proteopathies in order to determine their similarities and differences relative to the Aβ-type.
To this end, we are using organotypic slice cultures and a variety of genetically engineered mouse models of cerebral β-amyloidoses, tauopathies and α-synucleinopathies. To foster the translational and therapeutic aspects of our work, the results obtained from our mouse models are analyzed in comparison to those in the respective human patient samples.
A seminal finding from our group was the observation that misfolded Aβ can act as a seed to induce further Aß misfolding and aggregation in a manner that is strikingly similar to prion infectivity (e.g. Jucker and Walker, Nature Neurosci 2018). This finding provides a mechanistic understanding of recent findings in humans that inadvertent exposure to Aß seeds can induce iatrogenic cerebral Aβ deposition that, after prolonged incubation periods, is associated with clinical AD symptoms. This finding reinforces the importance of informed caution when working with Aβ and other proteopathic seeds. From a scientific perspective, the prion-like templating of Aβ misfolding implies that the most effective treatment to prevent Aβ deposition is to target Aβ seeds before the characteristic deposits of Aβ become detectable (Jucker and Walker, Nature Medicine, 2024). Indeed, we have been able to demonstrate such proof-of-principle prevention of Aβ deposition in the vasculature and brain parenchyma (Schelle et al., Ann Neurol 2019; Uhmann et al., Nature Neurosci 2020). The conformation-dependent templating of Aβ assemblies also implies that propagating Aβ assemblies may exhibit structural diversity and that therapeutic antibodies may target only conformationally distinct Aβ seeds. In a collaborative study, we were able to show a strikingly different conformation between Aβ deposited in the vasculature and in the parenchyma (Kollmer et al., Nature Comm 2019).
A long-standing key question in AD research is the relationship between Aβ deposition and the cognitive impairment. Aβ deposition in AD begins at least 20 years before the onset of clinical symptoms. In fact, Aβ deposition plateaus before symptoms first appear, making a direct neurotoxic effect of Aβ deposition unlikely. To investigate the link between Aβ deposition and neurodegeneration, we blocked Aβ production at different stages of Aβ deposition in mouse models. We identified two stages: a first stage characterized by the prion-like propagation of aberrant Aβ and a second, later stage where neurodegeneration became apparent, which progressed independently of Aβ deposition (Rother et al., Nature Comm 2022). This temporal uncoupling of protein aggregation and neurodegeneration resembles the bi-phasic development of prion diseases, further supporting the prion-like molecular properties of Aβ.
The finding that neurodegeneration progresses independently of Aβ deposition in later AD stages may provide a mechanistic understanding of why the clinical benefit has been limited in recent Aβ-immunotherapy trials (Jucker and Walker, Cell 2023). Earlier administration of the same antibodies, or a combination of Aβ antibodies with agents that target Tau, or neuroinflammation, may prove more clinically beneficial.
Full list of publications
Selected publications
Hofmann A, Häsler LM, Lambert M, Kaeser SA, Gräber-Sultan S, Obermüller U, Kuder-Buletta E, la Fougere C, Laske C, Vöglein J, Levin J, Fox NC, Ryan NS, Zetterberg H, Llibre-Guerra JJ, Perrin RJ, Ibanez L, Schofield PR, Brooks WS, Day GS, Farlow MR, Allegri RF, Chrem Mendez P, Ikeuchi T, Kasuga K, Lee JH, Roh JH, Mori H, Lopera F, Bateman RJ, McDade E, Gordon BA, Chhatwal JP, Jucker M, Schultz SA; Dominantly Inherited Alzheimer Network (2024) Comparative neurofilament light chain trajectories in CSF and plasma in autosomal dominant Alzheimer's disease. Nature Commun 18;15(1):9982 (Abstract)
Walker LC, Jucker M (2024) The prion principle and Alzheimer's disease. Science 385(6715):1278-1279 (Abstract)
Jucker M, Walker LC (2024) Evidence for the iatrogenic transmission of Alzheimer's disease. Nature Medicine 30(2):344-345 (Abstract)
Jucker M, Walker LC (2023) Alzheimer's disease: From immunotherapy to immunoprevention. Cell 186(20):4260-4270 (Abstract)
Rother C, Uhlmann RE, Müller SA, Schelle J, Skodras A, Obermüller U, Häsler LM, Lambert M, Baumann F, Xu Y, Bergmann C, Salvadori G, Loos M, Brzak I, Shimshek D, Neumann U, Dominantly Inherited Alzheimer Network, Walker LC, Schulz SA, Chhatwal JP, Kaeser SA, Lichtenthaler SF, Staufenbiel M, Jucker M (2022) Experimental evidence for temporal uncoupling of brain Aβ deposition and neurodegenerative sequelae. Nature Commun 13:7333 (Abstract)
Uhlmann RE, Rother C, Rasmussen J, Schelle J, Bergmann C, Ullrich Gavilanes EM, Fritschi SK, Buehler A, Baumann F, Skodras A, Al-Shaana R, Beschorner N, Ye L, Kaeser SA, Obermüller U, Christensen S, Kartberg F, Stavenhagen JB, Rahfeld JU, Cynis H, Qian F, Weinreb PH, Bussiere T, Walker LC, Staufenbiel M,Jucker M (2020) Acute targeting of pre-amyloid seeds in transgenic mice reduces Alzheimer-like pathology later in life. Nature Neurosci 23(12):1580-8 (Abstract)
Schelle J*, Wegenast-Braun BM*, Fritschi SK, Kaeser SA, Jährling N, Eicke D, Skodras A, Beschorner N, Obermueller U, Häsler LM, Wolfer DP, Mueggler T, Shimshek DR, Neumann U, Dodt H-U, Staufenbiel M, Jucker M (2019) Early Aβ reduction prevents progression of cerebral amyloid angiopathy. Ann Neurology 86(4):561-71 (Abstract)
Jucker M, Walker LC (2018) Propagation and spread of pathogenic protein assemblies in neurodegenerative diseases. Nature Neurosci 21:1341-1349 (Abstract)
Rasmussen J*, Mahler J*, Beschorner N*, Kaeser SA, Häsler LM, Baumann F, Nystrom S, Portelius E, Blennow K, Lashley T, Fox NC, Sepulveda-Falla D, Glatzel M, Oblak AL, Ghetti B, Nilsson KPR, Hammarstrom P, Staufenbiel M, Walker LC, Jucker M (2017) Amyloid polymorphisms constitute distinct clouds of conformational variants in different etiological subtypes of Alzheimer's disease. Proc Natl Acad Sci USA 114:13018-23 (Abstract)
Ye L*, Rasmussen J*, Kaeser SA, Marzesco AM, Obermuller U, Mahler J, Schelle J, Odenthal J, Kruger C, Fritschi SK, Walker LC, Staufenbiel M, Baumann F, Jucker M (2017) Abeta seeding potency peaks in the early stages of cerebral beta-amyloidosis. Embo Reports 18:1536-44 (Abstract)
Ye L*, Fritschi SK*, Schelle J, Obermüller U, Degenhardt K, Kaeser SA, Eisele YS, Walker LC, Baumann F, Staufenbiel M, Jucker M (2015) Persistence of Aβ seeds in APP null mouse brain. Nature Neurosci 18:1559-61 (Abstract)
Schweighauser M, Bacioglu M, Fritschi SK, Shimshek DR, Kahle PJ, Eisele YS, Jucker M (2014) Formaldehyde-fixed brain tissue from spontaneously ill alpha-synuclein transgenic mice induces fatal alpha-synucleinopathy in transgenic hosts. Acta Neuropathol 129:157-9 (Abstract)
Fritschi SK, Langer F, Kaeser S, Maia LF, Portelius E, Pinotsi D, Kaminski CF, Winkler DT, Maetzler W, Keyvani K, Spitzer P, Wiltfang J, Kaminski Schierle GS, Zetterberg H, Staufenbiel M, Jucker M (2014) Highly potent soluble amyloid-β seeds in human Alzheimer brain but not cerebrospinal fluid. Brain 137:2909-15 (Abstract)
Jucker M, Walker LC (2013) Self-propagation of pathogenic protein aggregates in neurodegenerative diseases. Nature 501:45-51 (Abstract)
Eisenberg D, Jucker M (2012) The amyloid state of proteins in human diseases. Cell 148:1188-203 (Abstract)

Hertie-Zentrum für Neurologie
Hertie-Institut für klinische Hirnforschung
Abteilung Zellbiologie Neurologischer Erkrankungen
Otfried-Müller-Straße 27
D-72076 Tübingen
Gisela Rose
Tel.: +49 (0)7071 29-81947
gisela.rose@uni-tuebingen.de
Dr. Jörg Odenthal
Tel.: +49 (0)7071 29-86862
Fax: +49 (0)7071 29-4757
joerg.odenthal@uni-tuebingen.de














