
Parkinson's disease (PD) is the second most frequent neurodegenerative disorder after Alzheimer's disease and affects about 1 to 2 % of individuals over the age of 65. The number is steadily increasing due to demographic changes in Western countries.
Clinically, most patients present with the cardinal motor symptoms of bradykinesia, resting tremor, rigidity, and postural instability but also suffer from a variety of non-motor symptoms such as autonomic dysfunction, depression, and hyposmia. However, the degree of progression shows a large variability with cognitive impairment as one major milestone of the disease.
Parkinson's Disease
Clinical Symptoms
Parkinson´s disease (PD) is the second most frequent neurodegenerative disorder after Alzheimer’s disease and affects about 1 to 2 % of individuals over the age of 65. The number is steadily increasing due to demographic changes in Western countries.
Clinically, most patients present with the cardinal motor symptoms of bradykinesia, resting tremor, rigidity, and postural instability but also suffer from a variety of non-motor symptoms such as autonomic dysfunction, depression, hyposmia and cognitive impairment.
Pathology
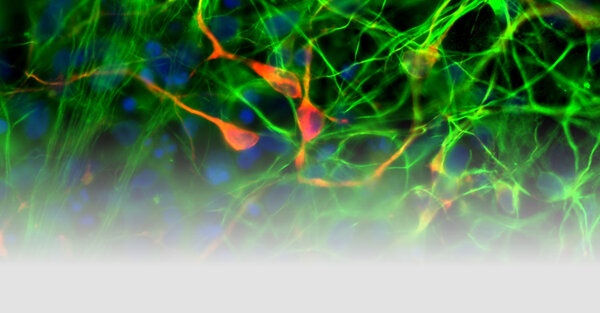
Underlying these clinical features is a progressive degeneration of dopaminergic neurons in the substantia nigra pars compacta (SNc), accompanied by an accumulation of eosinophilic intracytoplasmic protein inclusions, known as Lewy bodies and Lewy neuritis.
Prodromal Phase
Today we know that 40-60% of the dopaminergic neurons are already degenerated at the time when motor symptoms allow clinical diagnosis. This timespan in which neurodegeneration is proceeding without leading to classical motor symptoms is termed “prodromal phase of PD”. However, this phase is not inapparent. A variety of clinical non-motor symptoms may occur. They typically include, among others, constipation, olfactory dysfunction, sleep disorders (rapid eye movement behavior disorder and excessive daytime sleepiness), and neuropsychiatric symptoms such as depression and anxiety. The understanding of the prodromal phase of the disease may help to reliably identify at-risk individuals.
Milestones in the Disease Course
In the era where motor symptoms can be increasingly well controlled, dementia represents a key milestone in the course of PD. It is well known that, next to falls, dementia is one of the main predictors for the assignment to a nursing home and for death. However, the time course until reaching this milestone is highly variable. This calls for the identification of modifying factors which in turn might help to predict the course of the disease and possibly opens new therapeutic windows. Besides the quantification of clinical markers (neuropsychological scores, activity of daily living function), genetic variants and CSF profiles may help to define a high-risk group for Parkinson’s disease dementia at an early stage. These findings may have implications for future stratification and counseling of PD patients.
Genetics of Parkinson's Disease
Since twin studies in the 1980s failed to confirm evidence of familial aggregation, genetic factors were thought to play a minor role in the pathogenesis of PD. But nevertheless, PD patients with additionally affected relatives and PD families showing a typical pattern of inheritance were recognized. To date, we know of several genes causing either autosomal dominantly and autosomal recessively inherited forms of PD. More recently, advances in genetic technologies has allowed to focus on the contribution of gene variants to the development of the much more common sporadic form of PD. These variants are not directly disease causing but rather increase the risk for the development of PD. As the majority of these variants are not located in the coding regions of genes, their effect is most likely mediated by alterations of the regulation of gene expression.
The discovery of genes that are associated with Parkinson’s Disease has provided important insights into the molecular mechanisms underlying the disease. The major pathways to be discussed are mitochondrial and lysosomal dysfunction.
Therapy
Current therapy is primarily symptomatic without effect on the disease-causing mechanisms. However, with the identification of genes that are associated with Parkinson’s disease, specific pathways underlying the pathophysiology in subgroups of patients have been discovered. These pathways include e.g. mitochondrial and lysosomal dysfunction as well as inflammatory patterns and represent the basis for new disease-causing and disease course-modifying treatment strategies.
Focus of Research
Since Parkinson’s disease is a complex multifactorial disorder with a large variability in phenotypes and progression, our focus of research aims patient stratification according to imaging patterns, genetic architecture and, importantly, the underlying pathologic processes, possibly reflected by distinct profiles in patient biomaterials such as blood and cerebrospinal fluid. This in turn is a most needed prerequisite to introduce patients to pathway-specific milestone-related therapies.
In this context, special interest lies in genetically-associated forms of the disease such as patients carrying a mutation in the GBA or LRRK2 gene. Moreover, we focus on one of the most important milestone in the course of the disease, namely dementia. Next to pathophysiological aspects, we aim to evaluate risk factors and prodromal symptoms for the development of dementia as well as impact on quality of life.
Outpatient clinic for Parkinson's disease
The outpatient clinic for Parkinson’s disease covers not only the sporadic form of the disease but also atypical forms such as dementia with lewy bodies, multisystematrophie, progressive supranuclear gaze palsy, and corticobasal syndrome. Next to an accurate clinical diagnosis we focus on long-term evaluation and disease progression.
Consultation hours, contact persons and further information can be found on the page of the Parkinson's Outpatient Clinic of the University Hospital Tübingen.
A current list of all publications can be found here:
https://pubmed.ncbi.nlm.nih.gov/?term=Kathrin+Brockmann&sort=date